
Healthcare operations run smoothly only when patients, providers, and insurers are all on the same page about coverage. That’s where Benefit Verification in Salesforce Health Cloud comes into play. This powerful feature simplifies the process of checking a patient’s insurance coverage before they receive care, ensuring that both the patient and the provider avoid costly surprises. Traditionally, verifying benefits involved phone calls, emails, or faxed forms, leading to delays, confusion, and sometimes denied claims. With Health Cloud, the process becomes automated, transparent, and accessible in one place. By activating and configuring Benefit Verification, healthcare organizations can confirm insurance status, coverage details, and benefit limits directly within Salesforce—without juggling multiple systems or waiting endlessly for responses. This not only saves time but also builds trust, reduces billing issues, and helps providers deliver care confidently, knowing that payment is secured.
What Is Benefit Verification?
- In Salesforce Health Cloud, Care Benefit Verification is the process of verifying a patient's health insurance coverage and benefits, ensuring they have the necessary coverage for a specific service or treatment
- In Salesforce Health Cloud, Care Benefit settings allow you to manage and track a patient's health insurance coverage and benefits.
- Benefit Verification is the process of checking if a patient’s insurance is active and what is covered before they receive treatment.
- It helps avoid problems like denied claims, billing issues, or surprise costs for both the provider and the patient.
Why Is It Important?
- Imagine seeing a specialist (like a urologist for kidney stones) and assuming your insurance will pay, but later you find out your coverage was expired or missing.
- Without verification, the doctor might not get paid or you might get a bill for something you thought was covered.
- Duplicate claims, pre-authorization requirements, and outdated insurance info can delay care or payments and create lots of confusion.
How Does Health Cloud Make Benefit Verification Easy?
Traditional way
- The clinic or patient manually fills out forms and emails or faxes information to the insurance company.
- Waiting for a long time for a response, or not knowing the result, leads to delays and frustration.
With Health Cloud
- The process is more automated and can be done right inside Salesforce.
- You just need to set up and activate Benefit Verification in the settings.
Steps to Set Up Benefit Verification
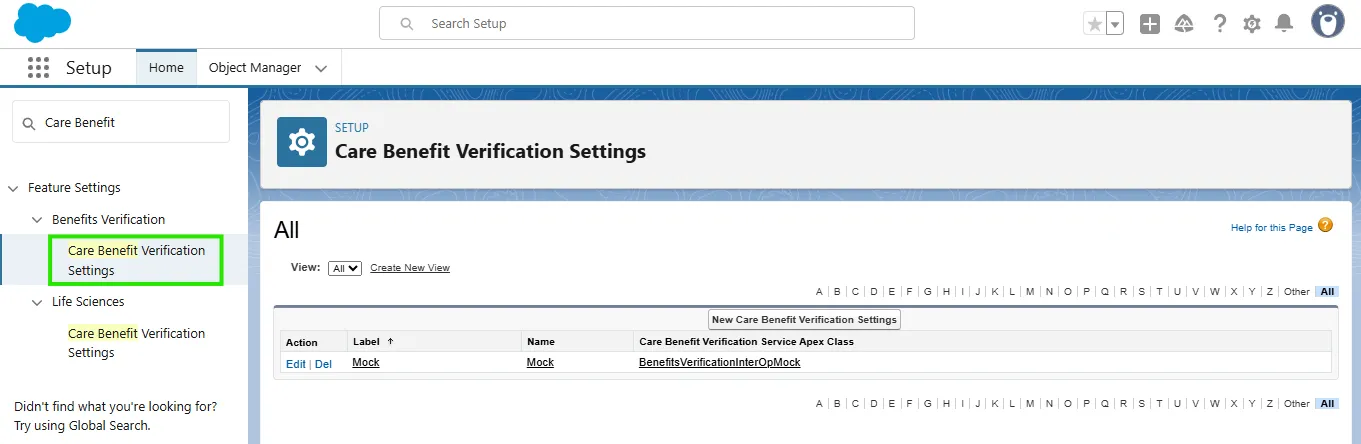
- Go to Setup, search for Care Benefit and then select on the Care Benefit Verification Settings option.
- If the Mock Care Benefit Verification setting is visible, click on it to review the configuration details (This setting was preconfigured as a placeholder (dummy) when the org was provisioned from Trailhead).
- In real-world projects, this API will connect Salesforce directly to insurance providers.
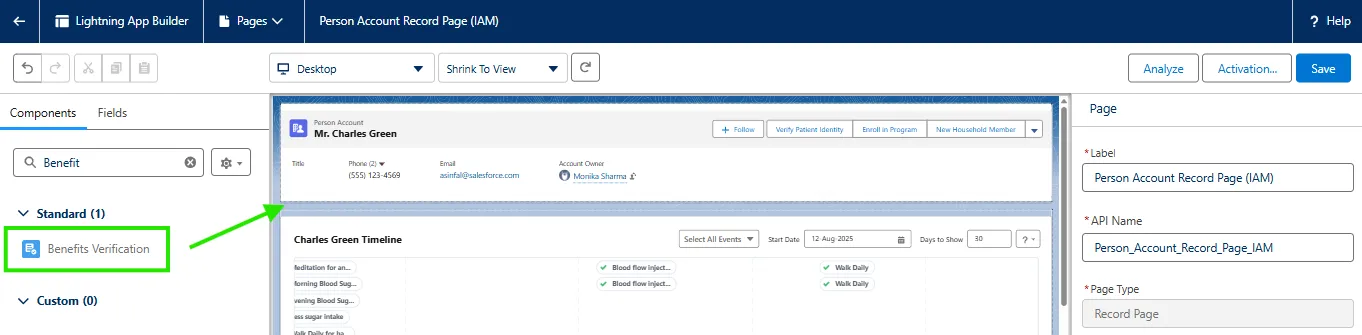
- Add the Benefit Verification component to an Account page layout (like on a patient's profile/account in Salesforce Lightning App Builder).
- Once added, open the patient/account record.
- Click the Benefit Verification section — you’ll see details like coverage, benefit plan, limits, and co-payment info.
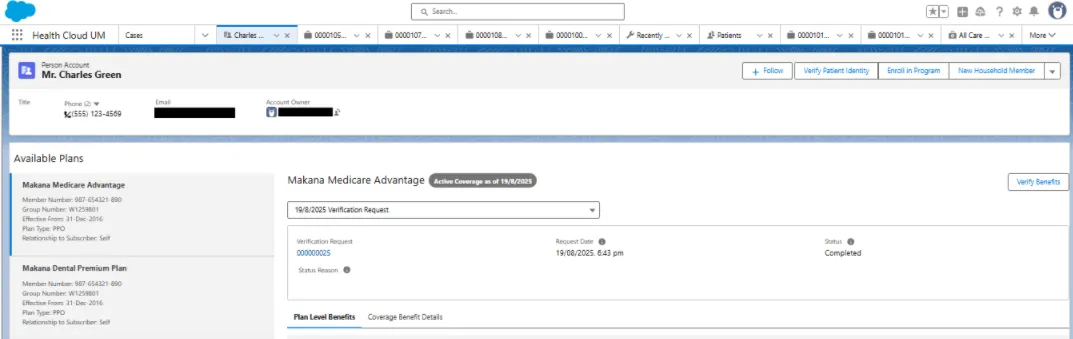
- Click Verify Benefits to check if the coverage is active. If verified, - you get a green light to continue with the care.
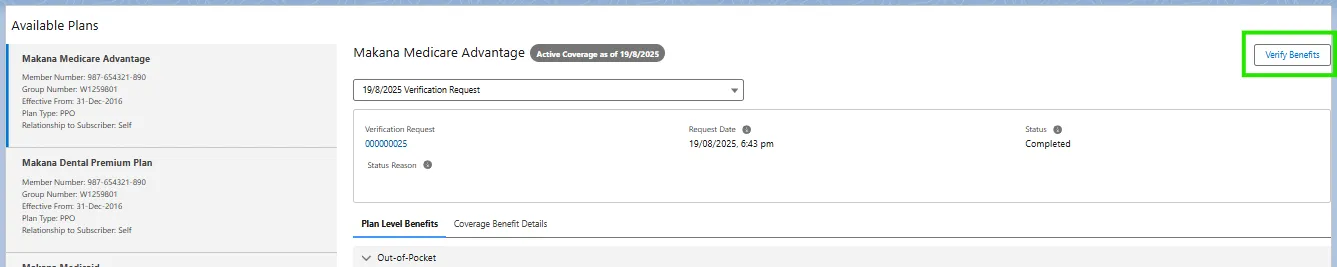
- After verify the benefit, it will look like the below figure.
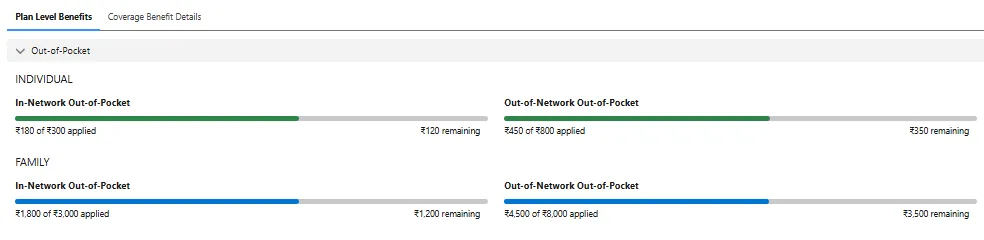
What Information Can You See?
- Plan-level benefit details (what’s included in the insurance).
- Limits on services or care types.
- Details like co-payments, allowances, and coverage amounts.
- Real-time confirmation of whether the patient’s insurance is ready and active for the proposed service.
Why Does This Matter in Everyday Clinic Life?
- Doctors and admin staff can quickly see if they’ll get paid for services—no need to trust just what the patient says.
- Patients aren’t surprised by bills or denials later.
- Less manual work and fewer delays compared to old email/fax forms.
- Everything is done in one screen—fast and easy.
Summary
Benefit Verification in Salesforce Health Cloud eliminates the manual hassle of checking insurance coverage by integrating the process directly into the platform. With real-time verification, clinics can confirm a patient’s active coverage, see benefit details, and prevent denied claims or unexpected bills. The result? Faster workflows, fewer errors, and a better experience for both patients and providers!